The pace of acute therapy and vaccine development for COVID have been dizzying. But even as we hope a route to bringing the pandemic under control is within sight, we’re now facing the possibility of another urgent public health emergency thanks to what’s known as long COVID, a group of symptoms that last long after the initial infection. With such a potential crisis looming, it is reasonable to ask what we are doing about it, and why treatments don’t appear to be forthcoming.
There are a few reasons why the long COVID story may pan out differently. Let’s take the first problem: long COVID is not a diagnosis itself. It encompasses many different problems, from blood clots and lung scarring to commonly recognised symptoms, with up to 82% still reporting symptoms like breathlessness, fatigue and brain fog 3-6 months after discharge from hospital.
Though this aspect of recovery has received much attention, most people are less aware that one in three COVID patients who leave hospital are back within three months of their apparent recovery – and one in ten are dead. Stark numbers and not many people are talking about them.
This complexity is a major challenge for those wanting to develop and trial treatments. One of the most important questions is the measure of health you wish to improve, or the primary endpoint. Each of the above diagnoses may need a different endpoint. If you have a clot you might die. If you have lung scarring you might be breathless and it might have changed your lung function. If your primary problem is fatigue, the most important thing may be improving the symptoms, getting you back to work or reducing the support you need.
Patient-led research has associated as many as 200 symptoms with long COVID. It is probable that some of these are not truly COVID-related, but how do you choose what to measure in a trial? Each time you add a new measurement in a trial you increase the size the trial needs to be to avoid false positive results. Compromises need to be made about what can be done versus what the patient might value as an outcome.
Recovery data
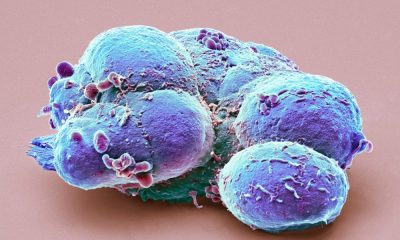
Next up is the underlying biology, of which we have a limited understanding. We know, for example, that clots form, but still not clearly why. We know that patients’ blood vessels are not normal, but not for how long this persists. And we know that some patients have prolonged inflammation, but we cannot predict who.
This makes it hard to choose therapies to trial and patients to include in those trials. It means we need to make some educated guesses who and when to treat, and with what.
Many patients recover, so should we enrol all patients when most of them will get better, pick out patients at higher risk of problems or wait until symptoms are established? No treatment comes without side-effects. We need to minimise the chances of harming someone who was going to get better anyway.
Added to this, the group we are studying may change with the advent of acute treatments and vaccines. Early reports suggest a younger population in the current wave.
This can have big effects on clinical trials. If you set a trial up to pick up a signal with an assumption of a third of people having long-term problems, if this reduces, then your trial might not be able to answer the question.
So what can we do about all this? The first thing is to run trials that are big enough for definitive answers and flexible enough to react to evolving knowledge, by including extra treatment arms if evidence changes.
The second is to have a mix of trials looking at different populations. Post-hospital patients are almost definitely at higher risk of problems like clots or scarring than those that were never admitted. Prevention is always better than treatment, so therapies aimed early in the disease course are important. The community patients who are living with persistent problems may need different trials.
Complex funding
The good news is that a lot of funding is being released to point at the problem, even if we don’t yet know the best areas to focus on. Another positive is that big trials like the vaccine studies and the Recovery trial (the world’s biggest clinical trial to identify treatments for people hospitalised with COVID), have shown we can do big trials at pace and scale.
Unfortunately, the current funding system is competitive, lacks co-ordination and doesn’t really reward collaboration. These big trials were the exceptions, not the rule. So we need pressure on funders and researchers to do things differently.
In the UK, we have set up an early example of the sort of trials we think we need, called Heal-COVID. It already has around 100 centres in the UK involved and puts into practice some of the ideas above. If you had told me before the pandemic that this type of trial could be set up in weeks, I would not have taken you seriously.
Despite this, the long-term nature of the problems mean it will be months before trials start to report and we need to explain to the public why. There are a lot of people out there desperate for something/anything and this will be fertile ground for charlatans and opportunists. So in the meantime, if patients are going to experiment they must always ask who benefits, make sure the treatments are at least safe, and take heart that a lot of patients are still on a journey of improvement. There remains hope.
Mark Toshner, Lecturer in Translational Respiratory Medicine, University of Cambridge
This article is republished from The Conversation under a Creative Commons license. Read the original article.