Even with three highly effective vaccines available in abundance throughout the country, the delta variant of SARS-CoV-2 continues to cause a large number of new infections, particularly in states where vaccination rates remain low. What’s more, as schools and businesses reopen and the holiday season approaches, another rise in infections may be on the way.
There is, however, some good news. Numerous medications, including fledgling and repurposed drugs, are accessible. For hospitalized COVID-19 patients, these new treatments, along with supportive care advances – such as placing some patients on their stomachs in a “prone position” – were helping bring down mortality rates before the Delta variant hit and are continuing to improve patient outcomes today.
As an infectious diseases physician and scientist, I have been working to find new treatments for patients since the pandemic’s beginning. Here’s a look at some of them, with one caveat: While these medications might help many patients, none substitute for the vaccine, which is still the best defense against the virus.
The right drug at the right time
COVID-19 has two main phases.
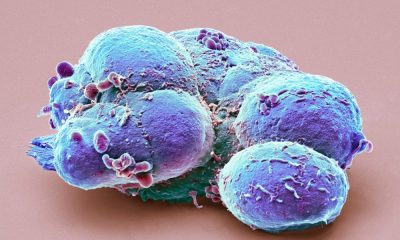
In the early stage of the disease, the SARS-CoV-2 virus replicates in the body; the virus itself causes illness. Within the first 10 days or so, the immune system eliminates the virus, but this process can cause collateral damage.
A second phase of the disease may kick in, which occurs when the patient has a disordered inflammatory response.
That’s why it’s critical to use the right treatment drug at the right time. For instance, an antiviral drug may help a patient with early and mild symptoms. But it’s not useful for someone on a ventilator after weeks in the hospital.
Conversely, patients in the ICU might benefit from an inflammation-reducing drug, which can prevent damage to organs such as the kidney and lungs; this damage is called sepsis. But the same drug used during the viral phase of disease might hamper a patient’s ability to fight off COVID-19.
Antiviral drugs
Three antiviral monoclonal antibody drugs authorized for use in the U.S. may keep the virus from infecting new cells by targeting the SARS-CoV2 spike protein. For outpatients with early COVID-19, these drugs reduce the risk of hospitalization and death. One of them – REGEN-COV – may prevent high-risk patients from getting sick.
These antiviral drugs might also help hospitalized patients whose bodies are unable to make antibodies on their own, either because of immune-compromising drugs or an impaired immune system from another condition.
One study that has not yet been peer reviewed shows that hospitalized patients with no natural antiviral antibodies had a reduced risk of dying after receiving one of these drugs. But that treatment is typically unavailable except through a compassionate-use program. To get the medication for a patient, a physician must ask both the drug manufacturer and the FDA for approval.
Another problem: Administering these antiviral drugs on a large scale is a challenge. Health care workers must give them shortly after the start of symptoms. The infusion or injection must be in a monitored setting. Patients may find it difficult to quickly access the treatment.
Mixed signals on remdesivir
One of these antiviral drugs, remdesivir, shows activity in the lab against a broad range of viruses, including coronaviruses like SARS-CoV-2. It works by blocking the virus from making more copies of its genetic material.
Two clinical trials performed early in the pandemic show that remdesivir shortens recovery time for hospitalized COVID-19 patients. A more recent trial suggested it reduced the risk of death. But two additional trials, one conducted primarily in low- and middle-income countries by the World Health Organization and another in Western Europe, did not show a clear benefit of remdesivir in hospitalized patients.
The medical community has interpreted the conflicting data in different ways. Remdesivir received FDA approval to treat COVID-19; both the Infectious Diseases Society of America and the National Institutes of Health recommend the drug for hospitalized patients. But the World Health Organization does not, at least outside of a clinical trial.
Anti-inflammatory drugs
Steroids like dexamethasone can broadly suppress the immune system and, in turn, reduce inflammation. For hospitalized patients, a regimen of dexamethasone decreased the risk of death, according to a February 2021 study published in the New England Journal of Medicine. The benefit was greatest for patients requiring the most respiratory support. But in the same study, for patients with no need for oxygen therapy, dexamethasone had no benefit, and in fact could be harmful.
IL-6 inhibitors
Steroids are a blunt instrument for immune suppression; other anti-inflammatory drugs affect the immune system more precisely. Critically ill COVID-19 patients with inflammation may have elevated levels of the IL-6 cytokine, a molecule the immune system uses to coordinate a response. For these patients, both tocilizumab and sarilumab – two drugs that block cells from responding to IL-6 – may reduce inflammation and decrease mortality when combined with dexamethasone.
JAK inhibitors
A class of drugs called JAK inhibitors – JAK being shorthand for a family of enzymes called Janus kinases – may also modify the body’s inflammatory response. They are used for some autoimmune conditions, including rheumatoid arthritis, and they block inflammation caused by IL-6.
Adding baricitinib, a JAK inhibitor, to remdesivir helped hospitalized patients recover faster than using remdesivir alone. Baricitinib also reduced mortality in hospitalized patients treated with dexamethasone. And, with the sickest COVID-19 patients, it helped reduce inflammation.
Of the drugs discussed, at the moment only the antiviral monoclonal antibodies are available for doctors to prescribe for patients who are not in the hospital. There is still a clear need for other drugs to help patients with early symptoms who are not hospitalized. Older medications that may be repurposed to treat these patients include inhaled corticosteroids and fluvoxamine, an antidepressant.
A dangerous trend
As for the now-controversial drug ivermectin: Preliminary results from one randomized, placebo-controlled trial did not show any benefit for COVID-19 treatment. Two more trials, also randomized and placebo-controlled, are underway.
For now, based on current evidence, ivermectin should not be used to treat COVID-19 patients. When used incorrectly, this drug could cause serious harm. Ivermectin has been approved for treatment of parasitic worms and head lice; but using it off-label to treat COVID-19 has resulted in overdoses and hospitalizations. Ivermectin toxicity can cause nausea, vomiting, diarrhea, low blood pressure, confusion, seizures and death.
The urgent search for COVID-19 treatments has highlighted the need for high-quality science. Early on, limited studies led some to believe that hydroxychloroquine would be useful for COVID-19. But over time, more rigorous research showed the drug to have no value for COVID-19 treatment.
Randomized, placebo-controlled trials – in which patients are randomly assigned to receive either the test drug or a placebo – represent medicine’s gold standard. They help doctors avoid the many sources of bias that can lead us to conclude a drug is helpful when it really isn’t. Going forward, it is this kind of research – and evidence – that is essential to finding new and effective COVID-19 treatments.
Patrick Jackson, Assistant Professor of Infectious Diseases, University of Virginia
This article is republished from The Conversation under a Creative Commons license. Read the original article.